Cardiology / Clotting Update
As I’ve had some news from various medical tests I thought it was time for an update. The heart attack I had almost 18 months ago came as a bit of a surprise. I had none of the usual risk factors, I was otherwise very fit, very healthy and had a pretty good lifestyle as far as heart health was concerned. So, after recovering from the heart attack itself, letting the stents settle in and getting used to the medication regime I started to ask some questions.
What Caused It?
What caused it was the obvious question. We knew from the Angiogram report that a large clot formed a 100% blockage of my Right Coronary Artery. That’s what caused the heart attack, but what caused the clot? Apparently, there wasn’t any significant narrowing of my artery and all other coronary arteries were in good condition and not blocked either. That was good news but it meant the clot itself was something of a mystery.
Most of the doctors and cardiologists just put it down to “one of those things”, bad luck and probably family history. However, looking at my family history, there wasn’t really that much that indicated a high prevalence of heart issues or heart attacks. What I did notice though was quite a high incidence of issues caused by clots. I wrote a blog post about this called ‘Is Clotting the Problem‘ back in December last year. I finished that blog post by saying
Lots to think about, lots of questions to answer, but maybe clotting is the issue. It’s an avenue that’s worth exploring if nothing else.
Investigating Clotting
So, I embarked upon a line of investigation to see if clothing was indeed the problem. This took longer than I expected. First I had to convince the right doctors to listen to me, and then finally managed to get to talk to a haematologist. Next, I had to convince the haematologist to run some clotting disorder tests for me. These were sent off to Cardiff for analysis, but somehow something went wrong, or they got lost so after quite a wait I had a second set of tests. These too were sent off to Cardiff and another long wait ensued.
Eventually, I did get the results of the tests and they showed that I did indeed have a hereditary clotting disorder. The actual letter stated:
These tests have confirmed that you do have the prothrombin 20210 genotype heterozygous variant in your blood. This will increase the risk of venous thromboembolism and arterial thromboembolism.
So, in other words, I do have a hereditary genetic mutation (also known as Factor 2 Leiden), which increases the risk of clots forming.
Answers
Maybe this was part of the answer I was looking for. Obviously, this in itself wouldn’t necessarily be enough to form the clot that caused the heart attack. As it’s hereditary, the risk had always been there. Maybe though, it was the final straw on that fateful day. A combination of me not getting any younger, a hard day training in the heat, dehydration, the Covid vaccine, the genetic mutation and plain old bad luck all came together to form a clot in just about the worst place possible.
Perhaps if any of those factors weren’t present I would have been OK.
Plans Going Forward
This new diagnosis of a clotting disorder raises questions of its own. First, is the fact that it’s a hereditary condition, so who else in my family needs to be tested for it? I guess the answer is anyone and everyone really, although I’m not 100% sure what the treatment would be for those that have it. I don’t think it is generally considered to be a high enough risk factor to warrant pharmaceutical intervention on its own.
The second is how my treatment should change. I had been on dual therapy anti-coagulation treatment. This is standard after a heart attack and stent insertion. Usually, you are put onto low-dose aspirin long-term (for life), along with a 12-month treatment of anti-platelets such as Ticagrelor. That was the case for me, but I had asked to remain on the Ticagrelor while I waited for the results of the clotting disorder blood tests.
Once those tests came back positive I then had to ask the question of how to proceed. I was half expecting to continue on the aspirin and also remain on the Ticagrelor, but at a lower dose. However, after a little bit of discussion, the haematologist and cardiologist have decided that dual therapy anti-coagulation isn’t necessary. Instead, I’ll stop the Ticagrelor altogether. I’ll also stop the low-dose aspirin and I’ll start taking Clopidogrel instead. Apparently, Clopidogrel is a slightly more powerful anti-coagulation agent than low-dose aspirin so may provide a marginal benefit.
So, that’s the plan. It does also mean that I can stop taking Lansaprozole as well as I was only taking that to protect my stomach from the aspirin and Ticagrelor. So, I’ll be swapping 3 of my medications for a single one. That sounds like progress I guess.
Echocardiogram
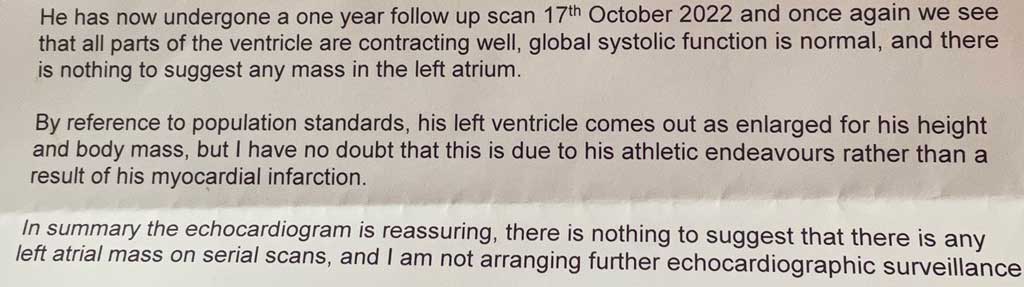
I also had an echocardiogram recently. I was due another as the original scan showed a possible mass in my left atrium. The results from that seem positive too. Here’s part of the echocardiogram report.
That sounds pretty good to me.
Back to Normal(ish)
I’m not completely back to ‘normal’. Although my previous normal wasn’t really normal I suppose. I am back to doing most of the things I want to be doing though. I’m swimming, cycling, running and kayaking (albeit quite a bit slower than before). I’m walking in the hills when I can, windsurfing when it’s windy and of course working, beekeeping and gardening when needed. I do still get some chest pains, I do still get tired more easily and I do get achy limbs quite bit (probably a side effect of the statins). I can live with that though. Next is to see how I tolerate the new pharmaceutical regime and to continue building my fitness.
I’d like to see if I can monitor my clotting ability too, but so far I’ve been told that’s not possible. Monitoring (if it’s possible) seems sensible to me as ideally, I’d like the drugs to counteract the clotting disorder just enough to stop clots forming, but not so much that I’m bleeding and bruising all the time. Surely some sort of monitoring makes sense just to make sure the drugs are doing what they should be?















All sounding good then .
As you know kia had an incident lately with her heart although no clot was detected however she had already been told she was at a higher risk of thrombosis from some tests she had and since your report back from the haematologist she is now waiting for some genetic testing.
Very interesting read Alan.
Alan interesting reading . As you know there has been a few members of our family with blood colts .. to now know about the These tests have confirmed that you do have the prothrombin 20210 genotype heterozygous variant in your blood. This will increase the risk of venous thromboembolism and arterial thromboembolism. I will ask my doctor about this to test for me !! & also tell my sisters & brothers & family about this ..
As my clot hit my eye & I lost some sight ..
Aspirin at first was my meds .
Then I started on Clopidogrel but I didn’t get on with it as it caused me severe headache in the front & couldn’t cope with the pain … severe bruising too on my arms chest & legs ..
So I am on modified release capsules Hard Dipyridamole 200g twice a day after food .. for life . Headache went within days ..
So if you have any issues with Clopidogrel may be worth an ask ..
Brenda xx
Thanks, I’ll bear that in mind – hopefully I’ll tolerate the Clopidogrel, but good to know there are other options if needed.
Al.